Long COVID, or Post-COVID Condition (PCC), continues to affect millions of Americans beyond the acute phase of infection. A new study published in PLOS ONE reveals a nationwide decline in physical, mental, and functional health among COVID-19 survivors, highlighting the urgent need for targeted care and recovery strategies.
Understanding the Burden of Long COVID
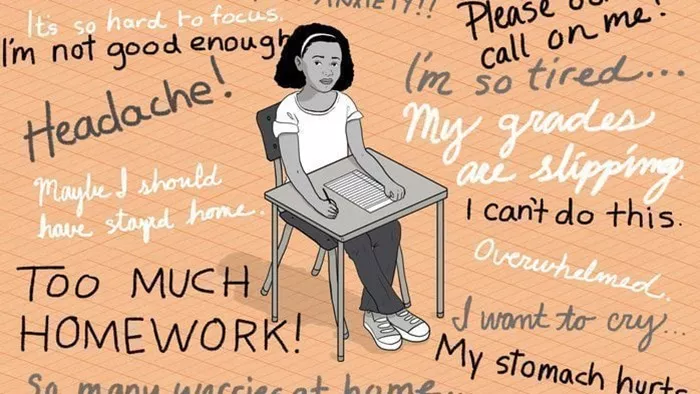
While the initial wave of COVID-19 infections has receded, many individuals continue to struggle with long-lasting symptoms such as fatigue, brain fog, dizziness, and pain. These persistent effects, collectively known as PCC, are estimated to affect nearly one-quarter of all U.S. COVID-19 survivors and often go overlooked as public attention shifts to infection prevention.
Although previous studies have hinted at the burden PCC places on individuals, few have comprehensively assessed its impact on health-related quality of life (HRQL) across large populations. This latest study provides new evidence to guide treatment and policymaking by identifying who is most at risk and how best to support them.
The Study
Researchers analyzed data from the 2022 Behavioral Risk Factor Surveillance System (BRFSS), a nationwide telephone survey led by the U.S. Centers for Disease Control and Prevention (CDC) that collects health information from adults. The study focused on individuals who tested positive for SARS-CoV-2 and excluded those diagnosed only at home or with incomplete diagnoses.
Participants were divided into two groups: those who reported PCC (defined as having symptoms that persisted for at least three months after acute infection) and those who did not. The researchers assessed HRQL using four self-reported indicators: overall health, mental health, physical health, and ability to perform daily activities. Additional factors such as demographic characteristics, comorbidities, and lifestyle behaviors (e.g., physical activity, smoking, sleep patterns) were also recorded.
To address missing data and control for confounding variables, the study employed advanced statistical methods, including multivariate logistic regression and random forest-based imputation. Survey weights and design adjustments were applied to ensure the results accurately reflected the adult U.S. population.
The study acknowledged some limitations, including reliance on self-reported data, which may be affected by recall bias or inaccuracies. Important variables such as vaccination status, timing and severity of initial COVID-19 infection, and medication use were not included in the dataset. Additionally, institutionalized individuals were not surveyed, and the HRQL questions were not standardized questionnaires, which may limit generalizability.
Key Findings
The study included 108,237 adults diagnosed with COVID-19, representing over 70 million Americans. Of these, 22.7% experienced PCC. Individuals with PCC were more likely to be female, middle-aged, obese, physically inactive, have poor sleep habits, and lower income.
Overall, 25.7% of individuals with PCC rated their general health as “fair” or “poor,” compared to only 15.5% of those without PCC. PCC patients also reported significantly more days with poor mental and physical health and greater difficulty with daily activities.
After adjusting for relevant variables, PCC was independently associated with a 39% increase in the likelihood of poor self-rated general health (adjusted odds ratio [aOR]: 1.39; 95% confidence interval [CI]: 1.28–1.52; p < 0.001).
Specific symptoms most strongly associated with poor health scores included dizziness upon standing (38%), mood disorders (36.3%), and musculoskeletal pain (34.1%). In contrast, symptoms such as loss of taste or smell were less likely to impact overall health.
Importantly, the association between PCC and reduced HRQL remained significant across all age groups and states, indicating a widespread and systemic burden.
Factors Associated with Poorer Outcomes
Among individuals with PCC, certain risk factors were found to increase the likelihood of poor health outcomes. These included:
- Late middle age (45–64 years; aOR = 1.47)
- Obesity (aOR = 1.27)
- Physical inactivity (aOR = 1.94)
- Abnormal sleep duration—either too little or too much (aOR = 1.55 and 2.15, respectively)
Chronic conditions such as diabetes (aOR = 2.29), heart disease (aOR = 2.01), and lung disease (aOR = 1.98) were also linked to a significantly higher risk of poor health. Socioeconomic factors—such as lower education, lower income, being unmarried, and Hispanic ethnicity—were independently associated with worse health outcomes as well.
Interestingly, while women with PCC were more likely to report poor health, gender was not a statistically significant factor after adjusting for other variables.
Geographic and Demographic Variations
The study identified significant geographic variation in the impact of PCC. States such as West Virginia, Kentucky, and Oregon reported the highest rates of impaired overall health, emphasizing regional differences in the long-term effects of COVID-19.
Another notable finding was the elevated impact of PCC on quality of life among individuals in late middle age. The burden appeared especially pronounced among those with prostate cancer, underlining the complex interaction between age, disease risk, and daily functioning.
Conclusion
This study provides compelling evidence that Long COVID is associated with substantial declines in health-related quality of life across the U.S. population. Individuals with chronic illnesses, obesity, low socioeconomic status, and unhealthy lifestyles are particularly vulnerable.
These findings underscore the need for a multidisciplinary approach to managing PCC, including long-term monitoring and personalized rehabilitation strategies. The researchers call for further studies to address data limitations and improve support for individuals affected by Long COVID.
As the acute phase of the pandemic fades, addressing the hidden burden of PCC will be essential for national public health planning and resource allocation.
Related Topics